
The Aging Athlete
Strength Training for Runners. Time to Get on Board.

Transfer of strength training to running mechanics, energetics, and efficiency
Many injuries occur when the body is fatigued¹, typically in the second half of games. Likely we most of us are familiar with the “too much too soon” training errors leading to injuries in endurance sports like running and cycling. As a medical practitioner working with athletes, I am always on the hunt for ways to make my patients more resilient, more efficient, and increase the body’s capacity to tolerate stress. Through my 20+ years in practice, I’ve seen the trends in running health come and go. We’ve seen the forefoot/rearfoot debates and debunks, foot pronation obsession, and pelvic drop myopics. I still give those mechanics a thought, but research is now prioritizing strength training, regardless of “poor” mechanics and foot strike.
Storniolo et. al.² studied 14 male runners (I’m aware of the small sample size) participating in an 8 week twice a week strength training program involving 45* leg press, squats, knee extensions (quads), knee flexions (hamstrings), and plantar flexion (calves) exercises. They found (not surprisingly given many other studies with similar findings) that strength training 2x/week improved metabolic economy in just 8 weeks. However, as much as myself and fellow medical practitioners would hope, it did not result in improved running mechanics.
While the study was a small sample size on only male runners, it is a reminder that strength training alone might not stop you from heel striking or a collapse in your knee.
Brad Neal et. al.³ found female runners with patellofemoral pain improved running mechanics by introducing running retraining (step rate, step width, mirror/video feedback), but not by strength training. However, both running retraining and strength training did have a positive effect on pain and function.
A takeaway from these studies is that strength training alone (and possibly rehab exercises) might not improve running technique and mechanics, however, it can improve metabolic economy which might be responsible for improving the body’s resiliency to tolerate higer loads related to running thus reducing the likelihood of becoming injured. Maybe it’s time we think about strengthening to improve running economy and reducing pain rather than correcting form and gait. Leave the mechanics correction to running retraining tactics and cues.
Limitations to these studies:
- Small sample size
- Does strength training improve endurance of posture, reducing the risk of fatigue causing poor mechanics
As we treat each client individually, we still approach running injuries from all sides- training errors, shoes, mechanics, strength/stability/fatigue, mobility, and recovery.
References:
1. Nagle K, Johnson B, Brou L, Landman T, Sochanska A, Comstock RD. Timing of Lower Extremity Injuries in Competition and Practice in High School Sports. Sports Health. 2017 May/Jun;9(3):238-246. doi: 10.1177/1941738116685704. Epub 2017 Feb 1. PMID: 28146414; PMCID: PMC5435151.
2. Storniolo JL, Fischer G, Bona R, Pinho A, Moorhead AP, Tartaruga M, Finatto P, Peyré-Tartaruga L. Transfer of strength training to running mechanics, energetics, and efficiency. Biol Sport. 2022 Jan;39(1):199-206. doi: 10.5114/biolsport.2021.102807. Epub 2021 Mar 6. PMID: 35173378; PMCID: PMC8805355.
3. Neal BS, Barton CJ, Gallie R, O’Halloran P, Morrissey D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta-analysis. Gait Posture. 2016 Mar;45:69-82. doi: 10.1016/j.gaitpost.2015.11.018. Epub 2015 Dec 29. PMID: 26979886.


The Aging Athlete
Learn what you can do to avoid losing muscle mass over 50.
From the NIH: “Sarcopenia is a syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength and it is strictly correlated with physical disability, poor quality of life and death. Risk factors for sarcopenia include age, gender and level of physical activity.” Sarcopenia affects Type II muscle fibers which are fast twitch fibers. Along with neurodegeneration that naturally occurs with aging, loss of fast twitch muscle fibers may increase the risk of falls.
From a performance level, we lose about 15% of our muscle mass between the ages 30-60 and 30% after the age of 60! These changes have been associated with decreased stamina, decreased power, decreased strength, and increased insulin resistance.
Ninety percent of glucose is stored in available muscle tissue. If an adequate amount of muscle tissue isn’t available for storage, the glucose turns into fat. Therefore, a loss of lean muscle mass can contribute to insulin resistance as the amount of muscle mass is inversely related to insulin resistance. Increase muscle mass, lower the risk of insulin resistance.
The good news is we can stop or slow down the rate of loss of muscle mass and strength by nutrition and specific resistance training.
Type II muscle fibers can be targeted by a form of exercise called eccentric loading. Eccentric loading occurs when a muscle is lengthening while it is contracting. Blood Flow Restriction has also been shown to increase Type 2 muscle fibers due to the reduced amount of oxygen available to the muscle during training.
Delayed Onset Muscle Soreness (DOMS) is soreness experienced 1-2 days following exercise. Bottom line is we want DOMS. DOMS is an inflammatory result of tension on muscles that results in the activation of satellite cells which, under the right conditions fuses with muscle fibers to hypertrophy. The “right” conditions require protein within 48 hours (ideally 30 min) after exercise, with an emphasis on the amino acid Leucine. Unfortunately, simple endurance exercise is not enough to contribute to activation of the satellite fibers required to create hypertrophy.
Leucine is available in eggs, chicken, lentils, turkey, pumpkin seeds, beef, salmon, and cottage cheese.
Lastly, research has shown that people over 50 need more volume than their younger counterparts to gain hypertrophy. The intensity wasn’t relevant. This means people over 50 can perform 6 sets at 40% 1 rep max to gain muscle mass and strength. For instance, to gain muscle mass in triceps, you can do 3 sets of push ups at moderate intensity and then 3 sets of tricep extensions. That will equal 6 sets (high volume) of exercise for the triceps.
In conclusion:
- Muscle mass and strength decrease after the age of 30
- Sarcopenia affects Type 2 (fast twitch) muscle fibers
- Eccentric loading can stop or delay sarcopenia by targeting Type 2 muscle fibers
- We should feel moderate soreness 1-2 days following training (DOMS)
- Protein that is particularly high in Leucine after training is necessary to help hypertrophy of muscle fibers
Dr. Jess specializes in creating training programs for muscle hypertrophy while taking into account the needs and abilities of the aging population as well as peri/menopausal women who are at an increased risk for tendinopathies.


Menopause and Tendinopathies
Learn why women in peri-menopause and menopause are at an increased risk for tendinopathies.
Perimenopausal and Menopausal Women and Tendinopathies
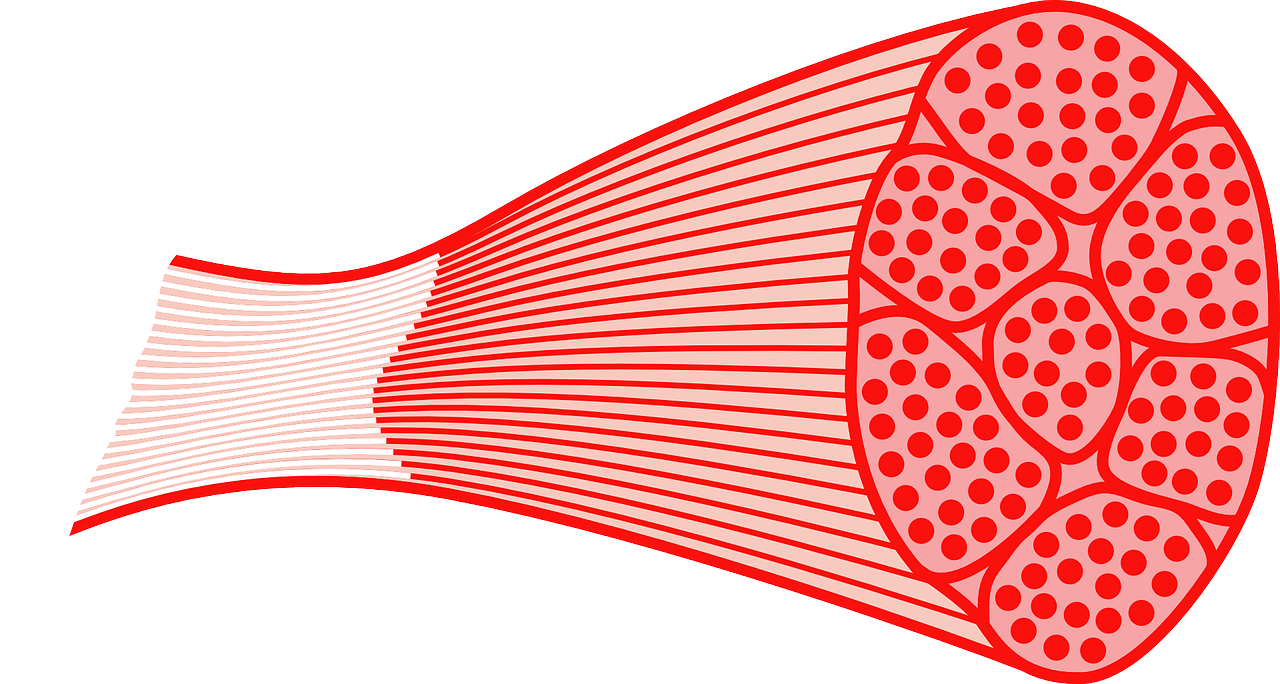
Tendons, which connect muscle to bone, store energy and transmit forces generated in the muscle, much like a rubber band. They are primarily comprised of collagen, a connective tissue that is both strong and tensile, protecting the muscle and bone from damage. Estrogen plays a key role in collagen synthesis
Estrogen drops significantly in peri-menopausal and menopausal women (and remains lower in post-menopause) which results in less collagen metabolism. The result is a stiffer, smaller tendon that is less able to regenerate and repair from activity and use.
Due to increased tendon stiffness and reduced capacity to repair, women with lower estrogen levels are more at risk for tendinopathies such as tennis or golfers elbow, achilles tendinopathy, and rotator cuff tendinopathies.
During perimenopause and menopause, active women need to increase activity at a slower, more gradual rate. In addition, inspite of the gradual loss of muscle mass as people age, perimenopausal and menopausal women are highly encouraged to increase lean muscle mass as well to help support tendon tissues.
Blood Flow Restriction has been shown to help grow lean muscle mass and improve tendinopathies. High load is essential to train a tendon to adapt and get stronger. However, high load is typically painful for an injured tendon. Blood Flow Restriction allows the patient to lift lighter loads while having the same effect as lifting heavy. For more on Blood Flow Restriction, click here.
